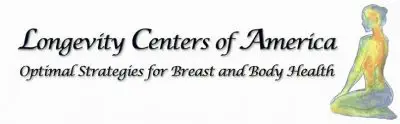
Normal Breast Scan
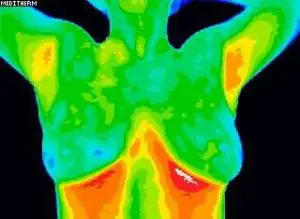
Abnormal Breast Scan
Breast cancer is a major health risk to all women. It silently grows uninterrupted for years. Early detection and prevention are key.
Digital Infrared Thermal Imaging takes a thermal picture to determine abnormalities or changes in the breast tissue. Breast Thermography can detect irregular patterns years before a mammogram. Best of all, Thermal Imaging is painless, non-invasive, and has no radiation.
DITI’s role in breast cancer and other breast disorders is to help in the early detection and monitoring of abnormal physiology and establish risk factors for the development or existence of the disease. When used with other procedures, the best possible evaluation of breast health is made.
This 15-minute non-invasive test is valuable for alerting your GP or specialist to the possibility of underlying breast disease. This test is designed to improve chances of detecting fast-growing, active tumors between mammographic screenings or when mammography is not indicated by screening guidelines for women under 50 years of age. A patient’s thermograms (breast images) are kept on record and form a baseline for all future routine evaluations. Use our convenient appointment scheduler to book your scan now.
DITI is especially appropriate for younger women between 30 and 50 whose denser breast tissue makes it more difficult for mammography to pick up suspicious lesions. This test can provide a ‘clinical marker’ to the doctor or mammographer that a specific breast area needs a particularly close examination. The faster a malignant tumor grows, the more infrared radiation it generates. For younger women, in particular, results from DITI screening can lead to earlier detection and, ultimately, longer life.
What it does: Breast thermography takes thermal images of the breasts and surrounding areas to aid in the early detection of breast cancer. Thermography assesses function rather than anatomically.
The principle: The procedure is based on the principle that chemical and blood vessel activity in both pre-cancerous tissue and the area surrounding developing breast cancer is almost always higher than in the normal breast. Since pre-cancerous and cancerous masses are highly metabolic tissues, they need abundant nutrients (blood flow) to maintain their growth. They increase circulation to their cells by sending out chemicals to keep existing blood vessels open, recruit dormant vessels, and create new ones (neoangiogenesis). This process increases the regional surface temperatures of the breast.
How it works: State-of-the-art breast thermography uses ultra-sensitive infrared cameras and sophisticated computers to detect, analyze, and produce high-resolution diagnostic images of these temperature and vascular changes.
Detection: The procedure is comfortable and safe, using no radiation or compression. By carefully examining changes in the temperature and blood
vessels of the breasts, signs of possible cancer or pre-cancerous cell growth may be detected years before being discovered using any other procedure. This

Healthy Breast Checkup
provides for the earliest detection of cancer possible. Because of breast thermography’s extreme sensitivity, these temperature variations and vascular changes may be among the earliest signs of breast cancer and/or a pre-cancerous state of the breast.
Research: Breast thermography has been researched for over 30 years, and over 800 peer-reviewed breast thermography studies exist in the index-medicus.
In this database, well over 250,000 women have been included as study participants. The number of participants in many studies ranges from 37,000 to 118,000 women. Some of these studies have followed patients for up to 12 years. Breast thermography has an average sensitivity and specificity of 90%.
Research Results: Studies show that:
- An abnormal infrared image is also the single most important marker of high risk for developing breast cancer
- Eight times more significant than a first-order family history of the disease.
- A persistently abnormal thermogram carries a 22x higher risk of future breast cancer.
- When added to a woman’s regular breast health checkups, a 61% increased survival rate has been realized.
- When used as part of a multimodal approach (clinical examination + mammography + thermography), 95% of early-stage cancers will be detected.
Infrared Scan: A positive infrared scan may indicate the presence of many different breast abnormalities, such as mastitis, benign tumors, fibrocystic breast disease, inflammatory breast disease, cancer, and others.
Just as unique as a fingerprint, each patient has a particular infrared map of their breasts. Any modification of this infrared map on serial imaging (images taken over months to years) can constitute an early sign of an abnormality. In patients without cancer, the examination results indicate possible future cancer risk. Consequently, without other positive tests, an abnormal infrared image gives a woman an early warning. By closely monitoring her breast health with serial infrared imaging, self-breast exams, clinical examinations, and other tests, a woman has a much better chance of detecting cancer at its earliest stage and preventing invasive tumor growth.
Unique Capability: Breast thermography’s ability to detect a pre-cancerous state of the breast, or signs of cancer at an extremely early stage, lies in its unique capability of monitoring the temperature variations and blood vessel alterations produced by the earliest changes in tissue physiology (function). At the earliest stages, a clinical thermographer can direct their client to “clean up their inner environment” and change temperature variations by alkalizing, detoxing, changing their diet, and teaching stress reduction techniques to reduce inflammation.
Thermography vs. other detections: Thermography assesses blood flow patterns, inflammation, and function. Mammography, Ultrasound, and Breast MRI assess densities and anatomical masses. Thermography cannot visibly pinpoint the location of an early-stage tumor. Mammography cannot see blood flow patterns and inflammation. Consequently, breast thermography is best used in conjunction with Mammography, Ultrasound, Breast MRI, and/or physical examination when there is a concern. Since it has been determined that 1 in 8 women will get breast cancer, we must use every means possible to detect cancers when there is an excellent chance for survival. Proper use of breast self-exams, physician exams, thermography, and mammography together provides the earliest detection system to date. If treated in the earliest stages, cure rates greater than 95% are possible.
Frequently Asked Questions (FAQ)
There are numerous websites that will give you further information. Among them is Thermology On-Line. Peace Of Mind
We try and make this service affordable for everyone. Prevention should be!
Insurance rarely (if ever) covers thermal imaging. However, you may use your Flex Spend dollars or Health Savings Account (HSA) money. If you still wish to check with your insurance company, call and inquire about thermography or thermal imaging insurance coverage for your specific condition. If you desire a Health Insurance Claim Form (HICFA), you will be given one with the codes already on the form. Fill out your personal information on the form and send it to your insurance company. There are no guarantees you will, in fact, be covered. You will still have to pay for the scan upfront. If your insurance covers the scan, a reimbursement check for the scan will be sent to you, or the balance will come off your deductible.
Please note: When referred by a Doctor, one copy of the scan results will go to the doctor that referred you, and one copy will come directly to you. You will be sent 2 copies of your report if you have no physician referral.
Some clients may wish to remain anonymous from the insurance company for personal reasons – or if they are changing insurance companies. We respect the confidentiality of each client.
Tell your doctor to do some research at Thermology On-Line (information, case studies). Also, there are downloadable studies at Healthy Breast Check-up https://www.thermologyonline.org (see radiation question above) call me at the Longevity Center, and I will send a booklet and lots of information to your doctor. Tell your doctor you have concerns with low-level radiation and how it affects DNA. There are over 800 studies on thermography. Hand her (or him) the 2004 Heyes study on radiation. If not thermography, ask for a different method (ultrasound, breast MRI, ductal lavage) as a substitute (see https://www.alternativemedicine.com on May mammogram article). In any case, thermography can be used in conjunction with a mammogram by assessing false positives or concurring with a sketchy mammogram.
It is up to us to get the word out about the benefits of Thermography and the dangers of Mammography to ALL doctors & radiologists. Here is a Fact Sheet for further information.
YES. Please visit https://www.thermologyonline.org for downloadable studies on the dangers of low-level radiation (2002 Brenner, 2003 Parisky, 2004 Heyes). Each time a woman gets a mammogram, she increases her chance of getting cancer by about five percent.
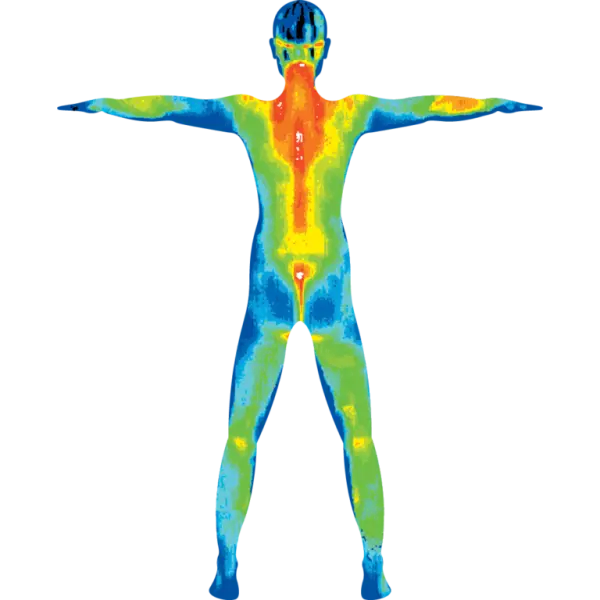
No. Thermography reads skin blood flow. In rare cases, inflamed liver, kidney, and colons appear on the stomach scan. However, thermal imaging can detect inflammation and pain (local or referred), chronic fatigue or fibromyalgia, thyroid concerns, lymph congestion, phlebitis, vasculitis, TMJ, dental pathology, sinus problems, and carotid arteries.
No, you do not need a referral if you are paying out of pocket or have a flex spend account. If you are submitting this procedure through an insurance company, they are more likely to reimburse you if referred by a Doctor.
Thermography has been around for almost 20 years. In the beginning, many doctors did not accept it due to a handful of untrained thermographers interpreting their own scans. A lot has changed since the early nineties, and thermal imaging is better than ever worldwide – including in Australia, Europe, and Asia. Scans are interpreted by board-certified MDs around the globe via the internet and are for medical use only.
As quickly as 24 hours, but in most cases 2-3 business days.
NO and NO! A picture is taken about four feet away to determine breast health. Pain and radiation-free!
After your initial breast scan, we suggest a second scan at three months to set a baseline. If there is no change from the first scan to the second, yearly scans are appropriate.
Mammography assesses anatomically (mass) and thermography assesses function (inflammatory).
Thermographic Scan Pricing
-
New Breast Scan – $249 (new to the Longevity Center or new to Thermography)
-
Comparative or Yearly Breast Scan – $179 (existing clients only)*
-
-
Region of Interest – $249 (head, abdomen, hips, knees, feet, hands)
-
New Breast and Region Scan – $319
-
Second Year Breast and Region Scan – $249
-
-
Women’s or Men’s Wellness – $349 (head, chest, abdomen, back)
-
Comparative Rescan – $299
-
-
Half body – $379, upper or lower
-
Comparative Rescan – $329
-
-
Full body – $479, head to toe
-
Comparative Rescan – $429
-
-
Add-on Additional Region – $70